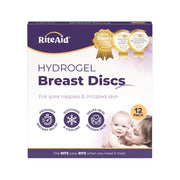
Hydrogel Breast Discs
Hydrogel Breast Discs
SKU:300131
In stock
Couldn't load pickup availability
Overview
Overview
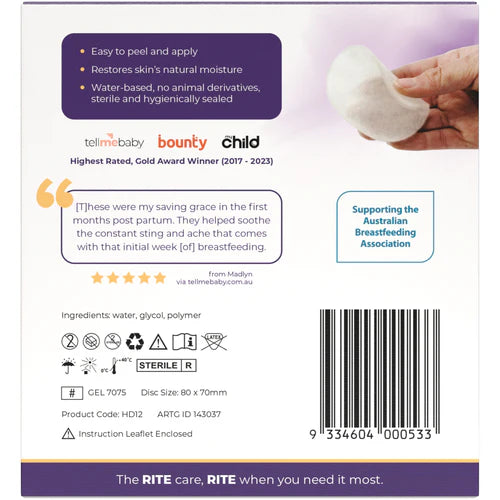
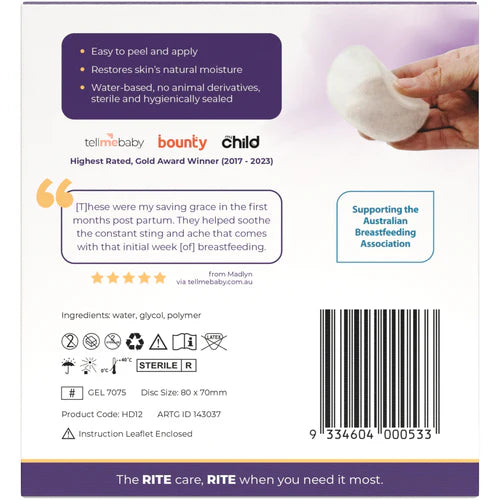
Experience relief with the award-winning Rite Aid Hydrogel Breast Discs, designed specifically for mums experiencing breastfeeding pain. These cooling hydrogel pads provide soothing comfort, promote healing, and protect sore nipples. Ideal for nursing mothers, our Hydrogel Breast Discs offer instant relief from breastfeeding discomfort, providing gentle care during breastfeeding.
- Easy to peel and apply
- Restores skin's natural moisture
- Water-based with no animal derivatives
- Sterile and hygienically sealed
Technical Specification
Technical Specification
User Guide
User Guide
Delivery and Returns
Delivery and Returns
- Delivery: Free within NZ on orders over $100 (excluding bulky items) or $8 standard shipping
- Returns: Accepted within 14 days of receipt with proof of purchase
- Some items are excluded from returns including sale items, hardware, car seats, prams, monitors and personal items - please click here for the full list.
Share this product
Recently Viewed Products
Related Blogs
Breastfeeding Basics and Tips
Understanding the Fundamentals of Breastfeeding Breastfeeding might seem straightforward, but many new moms find it challenging. Patience is essential, and being well-prepared can make the process smoother. Here, we break down the basics to help you get ready for this journey. The Three Stages of Breast Milk Colostrum: The First Stage When your baby is born, your body produces colostrum, a clear or yellowish liquid packed with nutrients, proteins, and vitamins. This small amount is perfect for newborns, helping to protect their digestive tract and immune system. Transitional Milk: The Second Stage Regular breastfeeding will stimulate the production of transitional milk, which appears around the third to fifth day. It looks like a mix of milk and orange juice, rich in lactose, fat, and calories. Mature Milk: The Third Stage By the second week, mature milk replaces transitional milk. This pale, sometimes bluish milk provides all the nutrients, fat, and proteins your baby needs, adjusting its water content in hot weather and boosting antibodies when needed. Achieving a Good Latch Proper latching is crucial to prevent discomfort. A good latch covers both the nipple and the areola and shouldn't be painful. Here’s how to ensure a successful latch: Positioning Your Baby Hold your baby tummy-to-tummy with your breasts, keeping their head aligned with their body. Mouth to Nipple Tickle your baby’s lips with your nipple or express a bit of milk to encourage the rooting reflex. When your baby opens wide, bring them to your breast. Ensuring Proper Attachment A proper latch involves the baby’s chin and nose touching your breast. If necessary, adjust the bottom lip to ensure it isn’t tucked in. Watch for a steady suck-swallow-breathe pattern. Trying Different Positions If you encounter difficulties, experiment with different breastfeeding positions like the football hold or side-lying. Consult a lactation consultant if needed. Maintaining Comfort and Milk Supply Relax and Feed on Demand Stay calm and relaxed to enhance milk production. Allow your baby to feed without time limits, ensuring one breast is fully drained before switching to the other. Recognizing Hunger Cues Signs of hunger include nuzzling your breasts, rooting, sucking on hands or clothing, and making lip-smacking noises. Crying is a late hunger cue. Feeding Frequency Newborns typically feed 8-12 times a day. Some may need to be woken up for feeds if they sleep for more than six hours. Patience and Persistence Breastfeeding takes time and practice. Be patient with yourself and your baby, seeking professional help if needed. With time, breastfeeding will become more natural and enjoyable for both of you. By following these tips, you can create a calm and successful breastfeeding experience, eventually making it look effortless.
Learn moreTrouble Shooting Breastfeeding Issues
When Breastfeeding Gets Tough: What You Can Do Many new mums set out hoping to breastfeed, but once baby arrives, things don’t always go as planned. Painful feeds, engorgement, latch troubles, low supply, clogged ducts, and infections – there are plenty of common hiccups that can make breastfeeding harder than you expected. Add in sleep deprivation, postpartum recovery, and all the well-meaning voices around you, and it’s easy to feel overwhelmed if feeding isn’t going smoothly. If you decide to supplement or switch to formula, there’s no shame in that – a fed baby and a supported mum are what truly matter. But if your heart is set on breastfeeding, the good news is most challenges can be worked through – and often, they’re only temporary. You've got this. Here’s a gentle guide to some of the common hurdles and how to help overcome them: 1. Engorged Breasts When your milk comes in a few days after birth, your breasts may suddenly feel hard, heavy, and tender – this is normal. It’s your body adjusting to baby’s needs. Engorgement usually settles down as milk supply begins to regulate, but it may crop up now and again if you go longer between feeds. What can help: Feed often, even if it’s just a little. If your breasts are too full for baby to latch, try hand expressing a bit first to soften the area. Cold compresses and gentle massage can bring relief. We stock some amazing inserts from Bare Mum which you can pop into your bra to help soothe the area. Some mums also swear by popping chilled cabbage leaves inside their bra between feeds – it’s an old remedy, but surprisingly soothing. 2. Latch Issues A bit of discomfort at the start of feeds is normal, especially in the early days. But if you're experiencing sharp or lasting pain, your baby might not be latching deeply enough. A shallow latch can press your nipple against the roof of their mouth, making it painful for you and less effective for them. What can help: Encourage a wide open mouth by gently rubbing under baby’s chin. Position them with their nose opposite your nipple, then bring them to you (not the other way around). A good latch usually means your baby’s mouth is wide, their chin is tucked into your breast, and your nipple is deep inside. If pain persists or your baby still can’t latch comfortably after a week or two, reach out to your midwife or a lactation consultant. Sometimes structural issues like tongue-tie can make latching difficult, and professional help can make all the difference. 3. Cracked or Bleeding Nipples It sounds scary, but many mums experience cracked or sore nipples in the first week or two. It can happen due to a shallow latch, overuse of a pump, or simply your skin adjusting to feeding. What can help: Use a nipple cream after each feed to soothe and heal. Hydrogel pads can bring instant cooling relief. Taking a mild pain reliever like paracetamol before feeds can help too. Most importantly, check baby’s latch – and ask for help if your nipples aren’t healing. Here are two of our favourite products to help you through: Pure Mama Nipple Butter and Silverette Cups these two in combination with each other should help you heal faster and stay protected. 4. Low Milk Supply It’s common to worry about supply, especially in those early weeks when baby seems to feed non-stop. But frequent feeding, short feeds, and night wakings are all normal and don’t usually mean you’re not making enough milk. True low supply is rare, but if your baby isn’t gaining weight or has very few wet nappies, it’s worth talking to your midwife or GP. Sometimes birth complications or certain medical issues can affect milk production. What can help: If baby is showing signs of dehydration, it’s important to get help quickly. Your healthcare provider may suggest medication or a feeding plan. If you’ve been given the all-clear but still want to increase your supply, try pumping between feeds, eating milk-boosting foods like oats and fennel, or treating yourself to some tasty lactation cookies or this delicious lactation blend. 5. Inverted or Flat Nipples You might not have thought much about your nipple shape before baby arrived – but inverted or flat nipples can make latching trickier. If your nipple pulls inward when gently pinched, it may be inverted. What can help: Most mums with inverted nipples are still able to breastfeed with the right support. Talk to your midwife or lactation consultant – they may suggest trying a nipple shield or using a breast pump briefly before feeding to draw the nipple forward. 6. Blocked Ducts A blocked duct feels like a hard, sore lump under the skin. It usually happens when milk isn’t draining well – perhaps due to a skipped feed or a tight bra. What can help: Keep milk flowing by feeding often on the affected side. Apply a warm compress before feeding and gently massage the lump toward the nipple. Most clogs clear within a day or two. 7. Mastitis If a blocked duct doesn’t clear or if bacteria enters through a cracked nipple, it can cause mastitis – a breast infection. You may feel feverish, achey, and have a red, painful area on your breast. What can help: Mastitis needs medical treatment, so see your GP for antibiotics. Keep feeding or pumping often – it might be sore, but emptying the breast helps you recover faster. Warm or cool compresses between feeds can ease the discomfort. 8. Thrush This yeast infection often begins in baby’s mouth and spreads to the breast. It can cause sharp, shooting pain and red, shiny, itchy nipples. What can help: Thrush won’t go away on its own, so you’ll need to see your GP for antifungal medication for both you and baby. It’s important to treat both of you at the same time to stop it from bouncing back. You Are Not Alone – and You’re Doing Great! Before baby arrives, breastfeeding can feel like it should come naturally – and for some, it does. But if you’re finding it hard, you’re not doing anything wrong. Many new mums face bumps in the road, and most find they only need support for a short time before things click into place. For others, despite trying everything, breastfeeding may not work out – and that’s okay too. You haven’t failed. Formula feeding is a perfectly valid option, and many babies thrive on it. What matters most is that your baby is fed, loved, and cared for – and you’re doing an incredible job. Don’t hesitate to ask for help – whether it’s from your midwife, GP, a lactation consultant, or another mum who’s been through it. And if you don’t feel listened to, keep asking. The right support can make all the difference ❤️
Learn morePostnatal Pelvic Floor Health: A Physiotherapist’s Guide
Bringing a new baby into the world is an incredible journey, but one that places big demands on your body - especially your pelvic floor.
Learn moreYour Guide to Antenatal Classes
At Dimples, we understand that preparing for the arrival of your little one can feel both exciting and overwhelming. That’s why we’ve teamed up with Grace Strange – Midwife and owner/founder of Antenatal Co.
Learn more